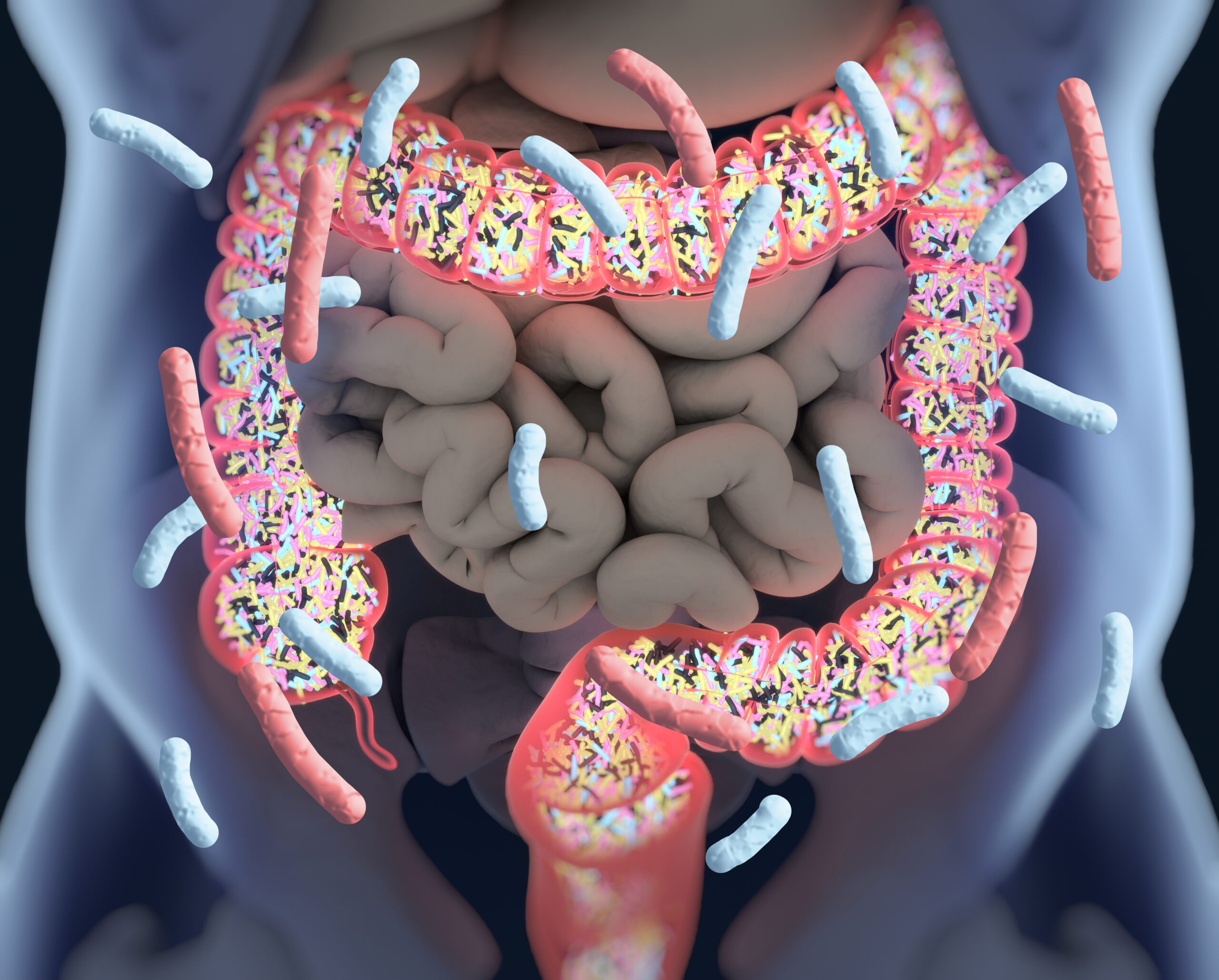
Microorganisms inhabit practically every surface of the human body, with the largest community residing in the large intestine. This dynamic ecosystem, known as the gut microbiome, is teeming with trillions of viruses, fungi, eukaryotes, protozoa, and most abundantly, bacteria. Each species features its own unique characteristics and functions that influence the health of the entire community.
The mutually beneficial relationship we have built with the microbes in our gut exemplifies a concept known as symbiosis—we provide a warm, nutrient-rich environment for them to thrive in; in return, they play a critical role in our digestion, nutrient absorption, immunity, and so much more.
The role of beneficial gut bacteria in digestion and metabolism
Beneficial bacteria in the gut help break down dietary fibres and other complex carbohydrates that our body cannot digest on its own, producing short-chain fatty acids (SCFAs) and other beneficial compounds in the process. These SCFAs (particularly one called butyrate) have well-established benefits for our health, such as reducing intestinal inflammation, maintaining a healthy gut barrier, and providing fuel for the cells in your gut1,2. And their benefits extend far beyond the gut—SCFA can help regulate your blood sugar, stimulate the production of certain hormones, and help regulate the immune system. In addition to their role in SCFA production, some bacteria in the gut contribute to the production of vitamins such as vitamin K and certain B vitamins that support our overall health.
The microbiome and immunity
Your immune system is a complex network of cells and organs that work to defend you against potential harm, including from disease-causing pathogens. We have evolved alongside our resident microbes, and they help train our immune system to fight off potential threats while tolerating the beneficial microbes and the products they produce3. This is a concept known as immune tolerance, and it helps maintain a healthy balance within the body.
In fact, studies in germ-free mice (those that are born and raised without any commensal bacteria) show that the absence of bacteria in early life can significantly impair the immune system, and this may contribute to certain autoimmune or inflammatory conditions and allergies later in life4,5. In humans, disturbances to the microbiome by things like antibiotics, dietary changes or damage to the gut barrier have been associated with certain inflammatory and autoimmune conditions3,6. Understanding how the gut microbiome interacts with the immune system is crucial for developing treatments for these and a wide range of other diseases.
Beyond the gut: how bacteria interact with our brain
There is a growing appreciation for the gut-brain axis and role that the microbiome plays in our mood and behaviour. Bacteria in the gut produce various compounds that send signals to the central nervous system to influence brain function and mental health7. So far, a lot of the research has focused on serotonin, a chemical that is widely known for its ability to regulate mood, happiness and anxiety. But it also plays an important role in the gut—roughly 90% of our body’s serotonin is produced and stored in the gut, where it helps regulate your digestion, gut inflammation and immune function8. Serotonin is produced by special cells in the gut lining, and this is stimulated by the SCFA butyrate.
Another mood-boosting chemical produced by certain gut bacteria is called gamma-aminobutyric acid (GABA). GABA has a calming effect that may improve sleep quality and help reduce anxiety and stress9, and changes in microbial GABA metabolism have linked to a range of mental health conditions10,11.
While there is evidence suggesting that signals from these and other neurotransmitters travel between the gut and the brain through a nerve called the vagus nerve12, more research is needed to disentangle the complex gut-brain communication network and its role in mental health and well-being.
What happens when the microbiome is disrupted?
Given its role across so many critical aspects of human health, it’s no surprise that imbalances in the microbiome, known as dysbiosis, can negatively affect our health. Dysbiosis has now been linked to numerous health conditions, including inflammatory disorders13, metabolic diseases like obesity and type 2 diabetes14, certain types of cancer15, and mental health conditions16. The research community is working hard to understand how we can restore the health of the microbiome in order to prevent or treat these conditions.
The take-away
The gut microbiome has generated a lot of interest in recent years, and for good reason. It influences virtually every aspect of our health, from digestion to immune function to mental health.
However, there’s still a lot we don’t know. The AHMB will provide researchers with access to thousands of different species from the human body (including the gut) so that we can continue to study the unique ways they influence our health.
References:
- Koh, A., De Vadder, F., Kovatcheva-Datchary, P. & Bäckhed, F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell 165, 1332-1345, doi:10.1016/j.cell.2016.05.041 (2016).
- den Besten, G. et al. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res 54, 2325-2340, doi:10.1194/jlr.R036012 (2013).
- Zheng, D., Liwinski, T. & Elinav, E. Interaction between microbiota and immunity in health and disease. Cell Research 30, 492-506, doi:10.1038/s41422-020-0332-7 (2020).
- Round, J. L. & Mazmanian, S. K. The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol 9, 313-323, doi:10.1038/nri2515 (2009).
- Cahenzli, J., Köller, Y., Wyss, M., Geuking, M. B. & McCoy, K. D. Intestinal microbial diversity during early-life colonization shapes long-term IgE levels. Cell Host Microbe 14, 559-570, doi:10.1016/j.chom.2013.10.004 (2013).
- Francino, M. P. Antibiotics and the Human Gut Microbiome: Dysbioses and Accumulation of Resistances. Frontiers in Microbiology 6, doi:10.3389/fmicb.2015.01543 (2016).
- Mansuy-Aubert, V. & Ravussin, Y. Short chain fatty acids: the messengers from down below. Frontiers in Neuroscience 17, doi:10.3389/fnins.2023.1197759 (2023).
- Jenkins, T., Nguyen, J., Polglaze, K. & Bertrand, P. Influence of Tryptophan and Serotonin on Mood and Cognition with a Possible Role of the Gut-Brain Axis. Nutrients 8, 56, doi:10.3390/nu8010056 (2016).
- Liwinski, T., Lang, U. E., Brühl, A. B. & Schneider, E. Exploring the Therapeutic Potential of Gamma-Aminobutyric Acid in Stress and Depressive Disorders through the Gut–Brain Axis. Biomedicines 11, 3128, doi:10.3390/biomedicines11123128 (2023).
- Valles-Colomer, M. et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology 4, 623-632, doi:10.1038/s41564-018-0337-x (2019).
- Braga, J. D., Thongngam, M. & Kumrungsee, T. Gamma-aminobutyric acid as a potential postbiotic mediator in the gut–brain axis. npj Science of Food 8, 16, doi:10.1038/s41538-024-00253-2 (2024).
- Kumar, A. et al. Gut Microbiota in Anxiety and Depression: Unveiling the Relationships and Management Options. Pharmaceuticals 16, 565, doi:10.3390/ph16040565 (2023).
- Bonaz, B., Bazin, T. & Pellissier, S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience 12, doi:10.3389/fnins.2018.00049 (2018).
- Caruso, R., Lo, B. C. & Nunez, G. Host-microbiota interactions in inflammatory bowel disease. Nat Rev Immunol 20, 411-426, doi:10.1038/s41577-019-0268-7 (2020).
- Fan, Y. & Pedersen, O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol 19, 55-71, doi:10.1038/s41579-020-0433-9 (2021).
- Gopalakrishnan, V., Helmink, B. A., Spencer, C. N., Reuben, A. & Wargo, J. A. The Influence of the Gut Microbiome on Cancer, Immunity, and Cancer Immunotherapy. Cancer Cell 33, 570-580, doi:10.1016/j.ccell.2018.03.015 (2018).
- Cryan, J. F. & Dinan, T. G. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience 13, 701-712, doi:10.1038/nrn3346 (2012).
The information on this website is not intended to diagnose, treat, or prevent any medical condition. See a full disclaimer here.